Community Leaders Elected to Board of Mission Hospice & Home Care
Leaders from across the San Francisco Peninsula and South Bay strengthen mission-driven nonprofit hospice
May 31, 2022 – Mission Hospice & Home Care, one of the region’s first nonprofit hospices, welcomes four new board members to its leadership team. Led by Chair Sally Bergman, the Mission Hospice board includes experts in healthcare strategy and management, oncology, internal medicine, pharmaceuticals, aging, finance, law, and fundraising.
Mission Hospice was founded by local residents in 1979, and is the only remaining independent, nonprofit hospice in the Peninsula and South Bay. Its board, staff, and volunteers all live locally, and the organization works closely with neighboring hospitals and community agencies.
“Thanks to our dedicated board, volunteers, and donors, Mission Hospice has provided compassionate end-of-life care for more than 40 years,” said Dolores Miller, RN, CEO of Mission Hospice. “While most hospice providers today are focused on profits, we remain guided by what the patient and family need. These new board members are committed to preserving the exceptional care that our community deserves.”
Mukund Acharya, Sunnyvale
Mukund Acharya is a social entrepreneur and advocate for healthy aging. He co-founded Sukham and founded Sandhya’s Touch, two organizations focused on quality of life for patients and families facing serious illness. Mukund is a volunteer at Stanford Hospital and School of Medicine, columnist for India Currents, and a board member of the Hindu Community Institute.
Stacy Blanchard, Redwood City
Stacy Blanchard is the Senior Managing Director, US West Strategy and Consulting Lead, for Accenture. She brings more than 20 years of experience in leadership, culture, and large-scale transformation.
Dr. Michelle Pezzani, Saratoga
Dr. Michelle Pezzani is a Medical Director at El Camino Hospital. She has more than 20 years of experience in hospital-based internal medicine and critical care, and more than a decade of experience launching and growing hospital services and programs. She also serves on the board of Next Door Solutions to Domestic Violence.
Dr. Beatty Ramsay, Hillsborough
Dr. Beatty Ramsay specializes in internal medicine, geriatric care, endocrinology, and diabetes. Over the course of his career, he has managed medical practices, as well as supervised and trained medical personnel.
###
About Mission Hospice & Home Care
Founded in 1979, Mission Hospice & Home Care is an independent nonprofit serving the San Mateo and Santa Clara County area with professional and compassionate end-of-life care and education. The organization has helped more than 17,000 patients and families live life to the fullest, offering comfort throughout the journey from a life-threatening diagnosis through death and bereavement. Generous support from the community helps Mission Hospice care for patients regardless of their medical coverage or ability to pay. More information is available at www.missionhospice.org
Mission Hospice and COVID-19
Across the globe, COVID-19 has disrupted lives and challenged us to adapt to difficult circumstances. While so much has changed, one thing that’s remained constant is our commitment to providing compassion, care, and kindness. Mission Hospice continues to support patients and families in the San Francisco peninsula and south bay with personalized, compassionate end-of-life care, grief support, and education. We have been serving this community since 1979, and we are here for you.
Patient care
The health of our patients, staff, volunteers, and community members is our priority, and we are monitoring and following the recommendations of the San Mateo County Health Department, California Department of Public Health, and Centers for Disease Control and Prevention.
Throughout the pandemic, we have continued to provide patient care in patients’ homes, facilities, and our hospice house, with all necessary precautions. As always, we have an RN available by phone 24/7. We are accepting new patients across all of our programs. If you or someone you know may be considering hospice, please call us at 650.554.1000 and ask to speak with our Clinical Outreach team.
Our teams are going above and beyond to provide care – through the pandemic, and even through wildfires and power outages. Read the story of one team here.
- 100% of our patient-facing staff is fully vaccinated.
- To minimize the spread of COVID-19 and to protect the health of our patients, our staff, and our community, our staff will ask screening questions in advance to determine if anyone in the family may have been exposed to COVID-19. Any family members exhibiting respiratory symptoms are requested to move to a separate room during our visit.
- Your nurse case manager will be checking in with you regularly to assess your needs. If you have any questions or concerns, please call us at 650.554.1000.
- Mission House patients and families should contact us directly for the latest visiting protocol.
Grief support
Many people, even those who haven’t lost a loved one, are experiencing grief at this time – and we have suggestions about how to manage grief during COVID. Our grief support groups and workshops have moved online, where we are reaching more people than ever. Check our Events calendar for the current status of all events.
We also offer individual grief support by phone and video. For information, please call us at 650.554.1000.
Community education
Our wide range of community education programs are now online, providing opportunities to learn and talk about how to live and die well. From our popular author and movie series to presentations from nationally recognized experts in resiliency, grief, and advance care planning, these virtual programs have become a resource for people around the world. Check our Events calendar for the current status of all events.
The pandemic has more people thinking and talking about advance care planning. We have moved our free Take Charge series online, where we can help people plan for their future care based on what matters most to them. Our Take Charge Toolkit and other advance care planning resources remain free and available to all on our Take Charge page.
Resources for our community
We urge everyone to follow the restrictions and guidelines in place. For all of us, and especially for caregivers, self-care is very important right now. You can find resources for caregivers here.
This two-minute video explains the importance of washing with plain soap and water.
Grief is more complex now, especially for those with underlying depression or anxiety. There is collective grief with the enormity of loss around the world to this virus, especially among the less privileged. Our bereavement coordinator Isabel Stenzel has written about grief in the time of COVID-19.
We also recommend these tips for managing the contagion of anxiety from Psychology Today, this BBC guide on How to protect your mental health, and this meditation for anxiety and stress from Love, Serve, Remember Foundation.
During uncertain times, it’s normal to want someone to talk to. For non-hospice-specific grief and/or loneliness, please consider these free resources for phone support:
- Institute on Aging’s Friendship Line: 800.971.0016
- Dignity Memorial’s Compassion Helpline: 866.649.9641
- Contra Costa County 24-hour Grief Hotline: 800.837.1818
- StarVista’s 24/7 Crisis Hotline: 650.579.
0350
Seeking donations
We are most grateful for the way our entire community has come together during this crisis. As we navigate into the future together, we are so grateful to our donors for their ongoing support, which is more important now than ever before.
Compassion and kindness
In the more than four decades since our founding, Mission Hospice has always been known for the compassionate care we provide – not only for our patients and families, but also for one another.
Social Work team helps families help themselves
From the Director of Social Work, Karri Kaiser, MSW
Social workers are often asked to explain what we do. My answer is that we help people learn to manage and solve challenges, both emotional and practical. Every day on the job is different, and that’s one of the things I love about social work at Mission Hospice. (Read “A day in the life of a social worker” for an example.)
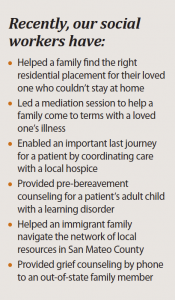
Our team provides emotional support, family mediation, life review, and grief counseling. We also help connect people to the financial, insurance, and community resources they need.

Social Workers Karri Kaiser, Meechal Hall, and Sara Martinez confer about how best to support a patient and his family members.
One of my roles as the Director of Social Work is to play matchmaker between family and social worker, leveraging individual interests and talents in a way that honors and respects each patient’s values.
 The diverse team of 15 social workers at Mission Hospice offers a breadth of expertise, including veterans’ affairs, conflict resolution, and bilingual support – we have social workers fluent in Spanish, Chinese, German, and Hebrew.
The diverse team of 15 social workers at Mission Hospice offers a breadth of expertise, including veterans’ affairs, conflict resolution, and bilingual support – we have social workers fluent in Spanish, Chinese, German, and Hebrew.
Mission Hospice thrives on teamwork. Our social work group meets regularly – often with other members of the care team – to discuss cases and work through challenges. We’ll discuss potential approaches, role play, and problem-solve, tapping the expertise and experience of the group as a whole.
Pre-bereavement and bereavement support is an important part of our job. I’m proud that in addition to our general drop-in grief support groups, we now also offer groups specifically designed for Spanish speakers, those who have lost a parent, those who have lost a spouse or partner, and young widows and widowers.
Sometimes people ask me how I can do this work, but it is truly a joy. We help people gain dignity and identify meaning, both in the past and in the present. By listening, we learn something from each patient about this road we will all go down.
Understanding spiritual care as part of hospice
From Mission Hospice & Home Care
Hospice care is known for including palliative medicine – the relief of symptoms and pain. But it also includes spiritual care; indeed, a number of studies and medical organizations recognize the importance of addressing patients’ spiritual pain as a part of total health care.
At Mission Hospice & Home Care, our professional hospice staff includes spiritual counselors Rev. Linda Siddall, Rev. Don Mulford, MK Nelson and Rachel Rosenberg, as well as spiritual care volunteers from a number of religious backgrounds. Our integrated compassionate care includes spiritual support expressly tailored to the patient’s needs and wishes.
While for some, spirituality equates with religion, spiritual care includes any beliefs, practices, and relationships that help people find meaning, comfort, and hope. This may include meditation, family and friends, writings, music, nature, and art.
Spiritual care has been a critical part of hospice care from the beginning. The founder of modern hospice, English physician Dame Cicely Saunders, considered it essential to address a patient’s physical, emotional, social, and spiritual pain: “Spiritual care is not an optional extra for the dying.”
Mission Hospice & Home Care recently held a professional development workshop to help our teams learn more about understanding and addressing patients’ spiritual pain. Richard Groves, a former hospice chaplain and cofounder of the Sacred Art of Living Center in Bend, Oregon, spent the day with medical staff, social workers, spiritual counselors and volunteers, sharing his extensive knowledge about identifying and addressing spiritual suffering and pain in patients and caregivers.
With input from medical professionals and a range of traditions, Groves has developed a Spiritual Health Assessment Tool to help caregivers and patients better understand – and address – the nature of spiritual suffering and pain. Essentially, this scale measures well-being from “extremely anxious” to “completely peaceful.”
Groves equates spirituality with self-awareness – a reflection that includes meaning, forgiveness, relationships, and hope. In The American Book of Living and Dying, he draws from Celtic, Tibetan, Egyptian, and other ancient traditions to provide perspective on humans’ most basic questions about life and death, and offers tools to help ease patients’ spiritual pain.
Groves predicts the coming of what he calls a “conscious dying” movement. “People don’t want to die the way their grandparents died,” he says. By contemplating our own death in advance, “we reap unexpected benefits for the rest of our lives.”
About grief
From Mission Hospice & Home Care
Grief is a normal response to loss. It is painful to lose someone you love, and the pain of loss can be profound. Each of us experiences grief differently. There is no right or wrong way to grieve. Grief can affect all aspects of our lives– psychological, physical, social, and spiritual.
Grief may involve many different emotions – sadness, loneliness, guilt, anger, helplessness, anxiety, fear, confusion, and relief. And while grief, for many, is intensely emotional, there are those who grieve quite deeply in other ways. Some may explore their grief and the issues and questions it raises through reading or writing. Others may grieve more actively by doing things that were important to their loved one or by becoming involved in a meaningful cause. It is important to remind ourselves that there are many ways to grieve; this prevents us from making judgments about how others are grieving, or how we, ourselves, grieve.
Grief may make it difficult to concentrate, remember things, and make decisions. This is a normal part of grief.
Grieving people may feel exhausted much of the time. It takes a great deal of energy to carry intense feelings of grief and learn to live without our loved one. It is common to experience a change in sleep patterns, a loss of appetite, and other physical symptoms. It is important to see a doctor before you assume symptoms are due to grief.
Grief prompts us to question and search for meaning. Our belief in the order and kindness of the world may be shaken. We may question our spiritual beliefs. We may ask, “why?” and ponder the meaning of our own death.
The process of grief offers choices. You can choose to grieve in a way that is right for you. Grief challenges us to find our unique strengths and offers the opportunity for transformation through personal growth and new meaning in our lives. We do not “get over” grief and return to “normal.” Grief changes us forever.
Because grief is a normal response to loss, it is not something that needs to be treated. But support groups and individual grief counseling can be a great source of support for those who are grieving or facing the death of a loved one.
Suggestions for healing
From Mission Hospice & Home Care
Grieving the death of someone close to you can be both physically and emotionally exhausting. Even the smallest tasks of daily living can be overwhelming. It is important to be good to yourself. Put aside what is unnecessary, and instead focus on what nourishes and restores you – and allows you to grieve.
Attend to your physical health and well-being. A healthy diet, plenty of rest, and regular exercise provide a good buffer against the stress of grieving. Do not neglect your routine health care. Consult a doctor if you experience any new symptoms.
It may be tempting to use alcohol or drugs to numb the pain of grief. This only postpones the necessary process of healthy grieving and can have adverse effects on your health.
Give yourself permission to grieve and the time to do it. Open yourself to every feeling that comes along. Give yourself both time alone and time with others whom you trust and who will listen. Be patient with yourself. Do not be discouraged if, at times, you feel that you are taking one step forward and two steps back. Such is the nature of grief. It is true that time does heal.
Give yourself permission to do the things that make you feel good, that comfort you, that give you respite from the pain of grief: a long walk, a good novel, a movie, dinner with a friend. Balance is important. Simple pleasure is good nourishment.
Share your loss with others. Find those who will listen without judgment. Talk about your loss with family and friends who are grieving the same loss. Talk about your loss with someone who is not affected by the loss. The company of others, each with a different perspective, can be valuable.
Trust your instincts and honor your needs. They will, no doubt, vary from day to day – even from moment to moment. You may have plans with someone and, at the last minute, have an overwhelming need to be alone. Allow yourself to cancel. The emotions of grief can be very unpredictable.
Although grieving is a normal response to loss, there are times when people need professional help with their grief. If your grief is seriously impacting other areas of your life (loss of relationships or a job), if you are engaging in self-destructive behaviors or having active suicidal thoughts, if after an extended period of time you continue to have no interest in life, or if others or you yourself feel that you need help – please find help. Seeking help is a sign of strength – not weakness.
If spirituality or religion are part of your life, you are probably well aware of how it can support and comfort you. Simple prayer can be sustaining. Religious and spiritual communities, beliefs, and rituals can all be a great source of strength to those who are grieving. It is not uncommon for loss to raise questions and doubts about one’s faith. If you are experiencing such doubts, find someone to talk about them with.
Remembering and honoring those who have mattered deeply to use remind us that, even though they are no longer physically present, our relationship with them continues. Our memories bring our loved ones into the present and remind us that they can continue to enrich our lives. Honoring our loved ones can help give meaning to a loss. Some ways we can do this are through rituals, artwork, writing, creating an altar or garden, or supporting a good cause.
Understanding the Medicare hospice benefit
 Former Medical Director Dr. Ken Barnes, Mission Hospice & Home Care
Former Medical Director Dr. Ken Barnes, Mission Hospice & Home Care
The first modern hospice was founded in London in 1967 by physician Dame Cicely Saunders, and the movement spread to the U.S. in the 1970s. Hospice gained significant momentum in this country with the 1982 creation of the Medicare Hospice benefit.
Along with more than 50 million other Americans, most of our patients are covered by Medicare. Understanding this benefit can help them take advantage of a wide range of services to support them – and their families – through the last months of life.
A patient can enter hospice care once a physician determines that the patient has six months or less to live and the patient chooses hospice over aggressive treatment. Medicare covers a broad range of services to manage pain and other symptoms, as recommended by the hospice team. The benefit covers care from hospice nurses and physicians, home health aides, social workers, chaplains, physical and occupational therapists, volunteers, dietary counselors, and other counselors, including those specifically trained in bereavement.
The Medicare hospice benefit also covers the rental of medical equipment such as wheelchairs or walkers, medical supplies, and prescriptions related to the hospice diagnosis. Medicare will pay for hospice care whether the patient is in her own home or in a facility such as a nursing home or board and care home. It will not, however, cover room and board, or the cost of private caregivers.
While most of our hospice patients are in treatment for less than thirty days, they can stay in hospice care as long as their six-month terminal prognosis remains certified by a physician. As patients’ needs or wishes change, hospice care may no longer be appropriate.
Here at Mission Hospice, our Transitions and Palliative Care programs helps ensure a continuum of care for patients who are not ready for hospice, whose health improves during hospice care, or who choose to seek additional treatments not covered by the hospice benefit. Our goal across our three programs is to provide pain relief, comfort, and emotional and spiritual support throughout the last months of life.
Many of our patients are covered by Medicare, but donations from the community help us serve people regardless of whether they are insured or can afford care. We are grateful for the support of our donors, who share our belief that everyone has the right to die pain-free and with dignity.
– from our February 2014 newsletter
Early referral to hospice means better quality of life
While most people know that hospice care is for the end of life, patients often ask us what this means in practice. When should a patient be referred to hospice?
Hospice care may be appropriate at any time during a life-threatening illness. Because the Medicare Hospice benefit (enacted by Congress in 1982) provides coverage for those thought to have six months or less to live, many people correctly think of this as the definition of hospice. We have found that the quality of life of patients and families is highest when the patient is in hospice care for as long as possible.
When the decision to start care is late, both patient and family can suffer unnecessarily.
Unfortunately, patients are entering hospice care later and later – a nationwide trend we are also seeing here at Mission Hospice. Across the country, more than half of all patients enter hospice care with fewer than three weeks to live, and 10% receive hospice care during the last twenty-four hours of life.
While our hospice teams provide valuable comfort, support, and symptom management (for example, to manage pain and shortness of breath) in these final weeks, patients and families often tell us that they wish they had known about or taken advantage of our services earlier.
The reasons for late referral are complex. Physicians can be overly optimistic about how long a patient might live. Both physicians and patients may want to fight the illness and not “give up,” an approach that can deprive the patient from addressing health care directives, mending relationships, or making financial arrangements at the end of life.
Studies have shown that hospice care is most effective when patients are with their teams for months, allowing them to build trusting relationships and participate in decisions about their care. Families have more time to prepare for the changes ahead. We as medical professionals have the opportunity to manage pain and symptoms sooner, helping to avoid crises and hospital stays.
Entering hospice care is not giving up – it is an opportunity for patients to truly live the last months of their lives. By addressing the possibility of hospice soon after a terminal diagnosis, the patient benefits from the physical, emotional, and spiritual care needed to ease his or her transition. We see every day that hospice care gives patients and their loved ones the opportunity to cherish their time together.




