Ron McKinney: Taking control with the End of Life Option Act
 By Joel McKinney
By Joel McKinney
After two decades of serious illness, in fall of 2021 our patient Ron McKinney chose to take aid-in-dying medication, surrounded by his family. His Mission Hospice team supported Ron and his family throughout the process, as we have with many others over the years who chose this path. His son Joel shares their family’s story.
More than 20 years ago, Dad was diagnosed with viral herpes encephalitis. It was life-altering for him – it affected his speech, memory, motor skills, communication, everyday life, and very existence. Overnight, it turned my mom into a long-term caregiver.
At the beginning, he was upset and frustrated. It’s a rare virus, and a lot of people don’t survive it. We’d all hoped that his speech and memory would improve, but they quickly plateaued, and he knew he wasn’t going to get back to where he had been.
Dad had seizures on and off for the rest of his life. As he became less and less active, his body really deteriorated. He took so much medication, some of which caused him to be groggy or dizzy.
It was hard to watch, but he did his best to put a smile on his face, laugh, and enjoy music and food. He simplified his life dramatically. He really looked forward to ice cream and the one beer he was allowed to have. He and mom handled it so gracefully.
In his last three years, his body failed him. He fell repeatedly and suffered broken hips, hip replacements, and stints in rehab. He was very tough, both physically and mentally.
Then my dad fell again, breaking his hip and his elbow. He had a high threshold for pain, but this was a different story. While he was in Sequoia Hospital recovering, a problem with his IV line led to his heart stopping, and I thought it was the end of the road for him. But they stabilized him, and within 24 hours he had started to talk and eat again.
 The surgeon explained what he wanted to do, and Dad said, “I’ve had enough. I’ve lived a good life and I don’t want to do this anymore. I’m done.” He said that part very clearly – he didn’t want any more surgeries, any more rehab, any more in and out of the hospital. We all agreed that we wanted to honor Dad’s wishes and not put him through any more suffering. We knew his quality of life was not going to get any better and would probably get worse – maybe a lot worse. He didn’t want that, and we didn’t want that for him.
The surgeon explained what he wanted to do, and Dad said, “I’ve had enough. I’ve lived a good life and I don’t want to do this anymore. I’m done.” He said that part very clearly – he didn’t want any more surgeries, any more rehab, any more in and out of the hospital. We all agreed that we wanted to honor Dad’s wishes and not put him through any more suffering. We knew his quality of life was not going to get any better and would probably get worse – maybe a lot worse. He didn’t want that, and we didn’t want that for him.
We asked the doctor what our other options were. How could we care for him without putting him through any more misery? The doctors at Sequoia told us about how wonderful Mission House is. It’s right in Redwood City where we live, and we all agreed that was the best place for Dad. Thank the Lord we were able to get him admitted within 48 hours. Mission House was amazing. Dr. Gary stopped by so often, communicated with us regularly – there were no surprises. He always answered all of our questions. We felt in really good hands with Mission Hospice.
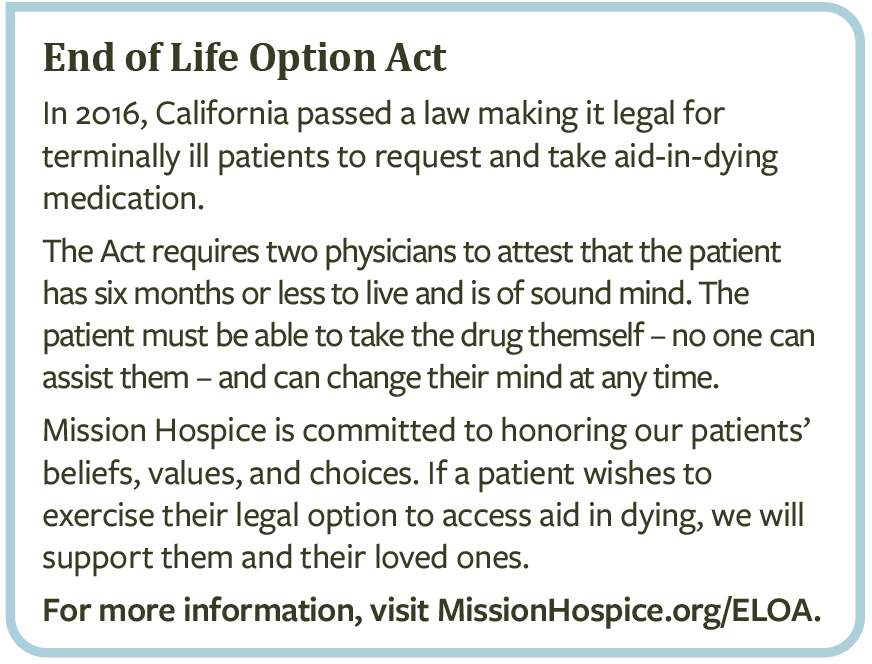
Dad was adamant in his desire to not go forward with long-term care or surgeries. Dr. Gary understood Dad’s wishes. We went back to the beautiful patio to chat, and he told us that Dad had to make decisions about how he was living every day. I was worried about Dad suffering. I knew there was aid-in-dying in other states. I asked Dr. Gary about this, and he explained California’s End of Life Option Act.
Dad knew that this was what he wanted, and we reassured him that we didn’t think God would judge him for it. Mission Hospice volunteer Paul Smith guided us through a number of conversations about spirituality, which was so helpful.
The law required another doctor to confirm that these were Dad’s wishes, and then we had to fill a prescription for the meds that would shut down his body. August 20 – that would be my dad’s last day with us. The days leading up to August 20 were the longest days of my life.
Still, it was good to have a date, and a plan. That allowed us to exhale and focus on spending as much quality time with Dad as possible. We sat with him, listened to music, watched movies, looked at photos. A lot of people came in from out of state – my brother and his wife, their son and daughter, my wife’s family – everyone. That was nice; it wasn’t a sudden goodbye. Even though Dad was still in a lot of pain, we could make each day as special as possible for him.
 The Mission House folks were all amazing. Anything we asked for, they made it happen. Dad loved to joke and try to make people laugh, and they were right there with him. We took him on walks around the ‘hood, spent time together as a family. We couldn’t have asked for a better place for him to spend his final weeks.
The Mission House folks were all amazing. Anything we asked for, they made it happen. Dad loved to joke and try to make people laugh, and they were right there with him. We took him on walks around the ‘hood, spent time together as a family. We couldn’t have asked for a better place for him to spend his final weeks.
When August 20 came, we all gathered in Dad’s room. We were able to tell him how much we love him, say our goodbyes, play his favorite songs.
Dad had been really lethargic. But as soon as the doctors walked in, he sprung up and took the medication. It felt like he was saving his strength for that moment. I think he didn’t want the misery or the pain to continue any longer. He was ready to be at peace.
The End of Life Option Act gave Dad a chance to do something about his life. He hadn’t had the power to do that for more than 20 years. For him to be able to make that choice, and for us to be able to support him, was empowering for all of us.
He took control.
I’ve been grieving my Dad for the last 20 years. Now I am at peace that he is no longer suffering, free of pain and burden, and strong and whole again.
